Peripheral Arterial Disease (PAD)
Peripheral Arterial Disease (PAD) is a common yet underdiagnosed circulatory condition that affects the arteries—especially those supplying blood to the lower limbs.
Dr Vascular Care
7/17/20252 min read
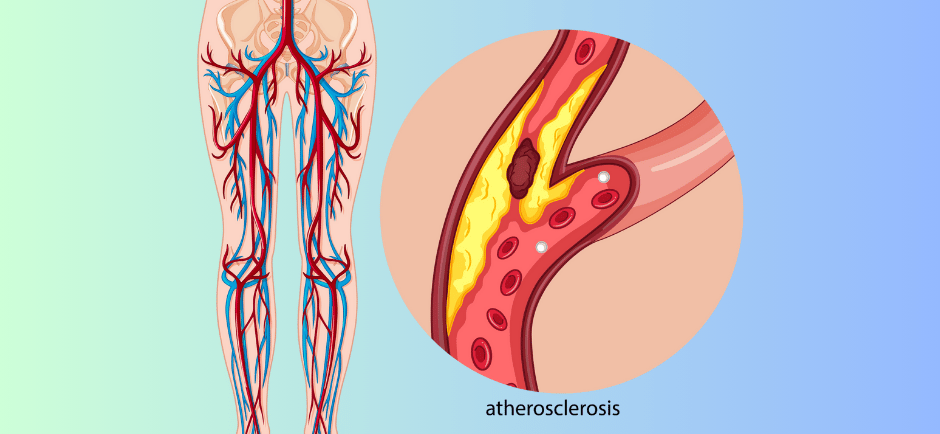
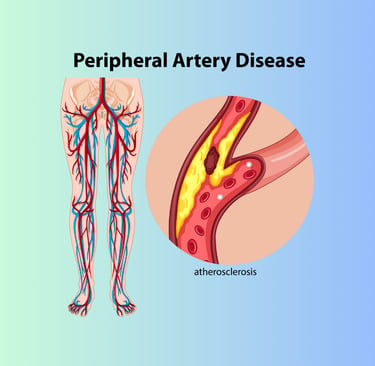
It occurs when fatty deposits (atherosclerosis) build up in the arterial walls, narrowing the arteries and restricting blood flow. PAD is not only painful and disabling in its advanced stages—it’s also a warning sign of widespread vascular disease that can affect the heart and brain.
Silent at First: Why PAD Often Goes Undetected
One of the most concerning aspects of PAD is that it can develop without any noticeable symptoms in its early stages. For many people, the first signs only emerge once the arteries are significantly narrowed. By the time symptoms appear, the disease may already be advanced. This silent progression highlights the importance of early screening, especially for people with risk factors.
When Symptoms Appear
PAD becomes more apparent as it progresses. The most common symptom is claudication—a cramping pain or fatigue in the legs or hips while walking, which typically subsides with rest. Other symptoms may include:
Numbness or weakness in the legs
Coldness in the lower leg or foot
Sores or wounds on the feet or toes that won’t heal
A change in skin color or hair loss on the legs
Slower toenail growth
In severe cases, pain may persist even at rest and be particularly noticeable at night when lying down.
Causes of PAD
PAD is primarily caused by atherosclerosis, the buildup of plaque (fatty deposits) in the arteries. This condition reduces blood flow and oxygen supply to the tissues. Other less common causes include:
Blood clots blocking the arteries
Inflammation of the blood vessels (vasculitis)
Injury to the limbs
Radiation exposure
Risk Factors
Certain factors increase your likelihood of developing PAD:
Smoking : The most significant modifiable risk factor
Diabetes: Doubles the risk and worsens complications
High blood pressure: Damages artery walls over time
High cholesterol: Contributes to plaque buildup
Age >50: Risk increases with age
Family history: Genetic predisposition to vascular disease
Obesity & Sedentary lifestyle: Slows circulation and metabolic function
Complications
Untreated PAD can lead to serious complications:
Critical Limb Ischemia (CLI): A severe blockage causing non-healing wounds, infections, and risk of amputation
Increased risk of heart attack and stroke: PAD is often a marker of systemic atherosclerosis
Poor wound healing: Especially in diabetic patients, increasing infection risk
Prevention
PAD is largely preventable through lifestyle changes:
Quit smoking: Reduces plaque progression and improves circulation
Exercise regularly: Walking programs can improve symptoms and promote blood flow
Eat a heart-healthy diet: Rich in fruits, vegetables, whole grains, and healthy fats
Manage diabetes, hypertension, and cholesterol: With the help of your healthcare provider
Regular check-ups are key—especially if you have risk factors. Screening may include a simple test called the Ankle-Brachial Index (ABI), which compares blood pressure in your ankle and arm to detect reduced circulation.
Diagnosis and When to Seek Help
PAD is often diagnosed through a combination of physical examination, blood flow tests (like ABI or Doppler ultrasound), and sometimes angiography to get a clearer view of the affected arteries.
If you experience leg pain while walking, wounds that don’t heal, or any signs of poor circulation in your legs or feet, it’s crucial to seek medical advice. Even if you don’t have symptoms, but fall into a high-risk group, early screening could prevent serious outcomes.
Takeaway
PAD doesn’t always come with warning signs, but its consequences can be serious. Don’t wait for symptoms to appear. If you’re over 50, diabetic, or have a history of smoking or heart disease—talk to a vascular specialist.
Early detection can save your legs—and your life.